The Effects of a Medial Heel Wedge on the Weight-Bearing Response of Hindfoot Valgus and the Total Weight-Bearing Responses of the Navicular and Talus Bones
Article information
Abstract
OBJECTIVES
Medial heel wedges are commonly prescribed to manage the weight-bearing response of hindfoot valgus and the total weight-bearing responses of the navicular and talus bones. Previous studies have reported that a medial heel wedge is effective in the management of musculoskeletal injuries. However, it remains unclear the effect of a medial heel wedge on the weight-bearing responses of footarch bones in vivo. To clarify the effects of a medial heel wedge on the weight-bearing response of hindfoot valgus and the total weight-bearing responses of the navicular and talus bones is necessary to understand how best to treat musculoskeletal injuries clinically. The purpose of our study was to clarify the effects of a medial heel wedge on the weight-bearing response of hindfoot valgus and the total weight-bearing responses of the navicular and talus bones.
METHODS
Twenty-five healthy males were analyzed. We obtained MRI scanning of the right foot under non-loading (NL) and full weight-bearing (FW) conditions. Participants wore two insole types, a flat insole and a medial heel wedge. To evaluate the weight-bearing response in hindfoot valgus, the hindfoot alignment view (HAV) was measured. We also measured navicular and talus bone positions and calculated the total positional changes of the navicular and talus bones (ΔTPCN, ΔTPCT) from the vertical and medial displacements using the Pythagorean theorem.
RESULTS
Significant interactions were observed with the HAV. Under both NL and FW conditions, the HAV was smaller on the medial heel wedge than on the flat insole. In addition, the ΔTPCN was significantly smaller on the medial heel wedge than on the flat insole. However, no significant differences were observed for ΔTPCT.
CONCLUSIONS
Our results suggest that use of a medial heel wedge decreases hindfoot valgus values under both NL and FW conditions and stabilizes the total weight-bearing response of the navicular bone.
Introduction
The human foot structure functionally deforms to absorb the impact of the foot [1]. When an axial load is applied, the weight-bearing response of hindfoot valgus and the total weight-bearing responses of the navicular and talus bones are functionally linked together to absorb the load [2-4], which are important processes for absorbing loads [4-6].
On the other hand, an excessive weight-bearing response of hindfoot valgus may apply mechanical stimulation to posterior tendons and cause further microtrauma [7]. Previous studies have reported that an abnormal total weight-bearing response of the navicular and talus bones, such as increased mobility or changes in the ratios of vertical to medial displacement, are likely associated with injuries [8]. Therefore, using foot orthoses to control an excessive weight-bearing response of hindfoot valgus and abnormal total weight-bearing responses of the navicular and talus bones are essential considerations in the clinical setting.
Medial heel wedges are commonly prescribed to manage the weight-bearing responses of foot-arch bones and musculoskeletal injuries [9]. Previous studies have reported that a medial heel wedge is effective in the management of musculoskeletal injuries [10]. Furthermore, previous studies have shown that the use of a medial heel wedge can cause biomechanical changes in the ankle, knee, and hip joints and support the promotion of movement [11-13]. From the abovementioned, it is considered that biomechanical changes in the entire lower limb caused by the use of medial heel wedge contribute to injury prevention [14]. Conversely, the effects of a medial heel wedge on the weight-bearing of foot arch bones are unknown because performing direct measurements of the weight-bearing responses of foot-arch bones in vivo has been challenging. Foot orthosis is prescribed to improve foot function based on the assessment of foot function [13,15,16]. Furthermore, previous studies have reported that foot function influences the entire lower limb function [17,18]. Therefore, the detailed effects of a medial heel wedge on the weight-bearing of foot arch bones will be fundamental knowledge for the management of musculoskeletal injuries of the lower limb.
Recently, positional magnetic resonance imaging (pMRI) has been developed. In a previous study, we investigated the weight-bearing response of hindfoot valgus and the total weight-bearing responses of the navicular and talus bones using pMRI [2]. This method can also be used to determine a medial heel wedge’s effectiveness at influencing the weightbearing responses of the foot-arch bones. The present study aimed to clarify the effects of a medial heel wedge on the weight-bearing response of hindfoot valgus and the total weight-bearing responses of the navicular and talus bones.
Methods
This study was approved by the University of Tsukuba Physical Education Research Institutional Review Board [Task No. PE019-54].
Participants
Twenty-five male volunteers participated in this study. Participants were recruited from University of Tsukuba students through e-mail and information sharing. All participants were free of lower-extremity pain and subjective symptoms interfering with walking or sports-related activities and had no history of serious injuries or operative treatments. All participants gave written informed consent to the purpose and procedures of this study before participating. The average ± standard deviation (SD) of the participants’ ages, weights, and heights were 23.24 ± 2.10 years, 69.04 ± 5.96 kg, and 173.54 ± 5.57 cm, respectively.
Protocol
Our study was comprised of two sessions, including a flat insole session and a medial heel wedge session, for each participant, with at least one day between sessions. Participants wore either the flat insole or the medial heel wedge during the 1st session and then wore the other type of insole during the 2nd session. This order was randomly assigned. In both sessions, MRI was conducted immediately after the participants wore the insole. During each session, MRI scanning was performed under two conditions: nonloading (NL) and full weight-bearing (FW).
Insole Types
The two insoles were a combination of a flat cork insole and silicon heel wedge. A heel wedge was not used for flat insoles, whereas an elevation of approximately 4° was used for the medial heel wedge. The length, width, and thickness of the medial heel wedge were 5.5 cm, 8.0 cm, and 1.0 cm, respectively. A heel wedge was attached to the inner heel section of the flat cork insoles.
Magnetic Resonance Imaging Procedure
Imaging was conducted using a positional MRI system (0.25 T G-scan, Esaote, Genoa, Italy). We scanned the right foot in two different conditions: NL and FW [19,20]. The applied pMRI protocol included the following sequences: scout—slice thickness, 10 mm; field of view, 280 × 280 mm; and scan time, 39 seconds and three-dimensional—TE, 4 ms; TR, 8 ms; FA, 75; field of view, 350 × 350 × 280; matrix, 208 × 208 × 122; and scan time, 8 minutes 6 seconds. Under the NL condition, the talocrural joint was positioned at a 90° angle to the long axis of the tibia. Under the FW condition, participants were positioned in a two-legged stance and instructed to stand with pressure equally distributed on the heel and anterior plantar sole. Under both NL and FW conditions, the foot was oriented vertically to the scanner bed, with the participants’ feet at the same width apart as that in a relaxed standing position [2]. A careful examination was conducted to ensure that there would be no differences in foot positions between the conditions.
Image Analysis
For image analysis, we used commercially available software (ITK SNAP, www.itksnap.org) [21]. The hindfoot alignment view (HAV), navicular bone height (NH), talus bone height (TH), medial navicular bone position (MNP), and medial talus bone position (MTP) were measured. The methods for obtaining HAV, NH, TH, MNP, and MTP measurements have previously been described in detail [2,22-24].
To measure the HAV, we used coronal images of the foot, in which the most central image through the distal tibial shaft was shown. The image was identified as the one in which the tibial shaft diameter was maximal, with a sharply defined tibial cortex [2,22]. First, we drew two lines which connects two pairs of points on the cortex of the distal tibia. We set the lower line above the distal tibial spread adjacent to the ankle joint and the upper line approximately 2.0 cm above the lower line. We drew the distal tibial shaft axis which connects the midpoints of two lines <Figure 1> (a). Then, we scrolled through the coronal images to find the lowest point of the calcaneus <Figure 1> (b). Finally, we measured the distance from the tibial axis to the lowest point of the calcaneus as the apparent moment arm <Figure 1> (c). Positive values signified hindfoot valgus, and negative values signified hindfoot varus.
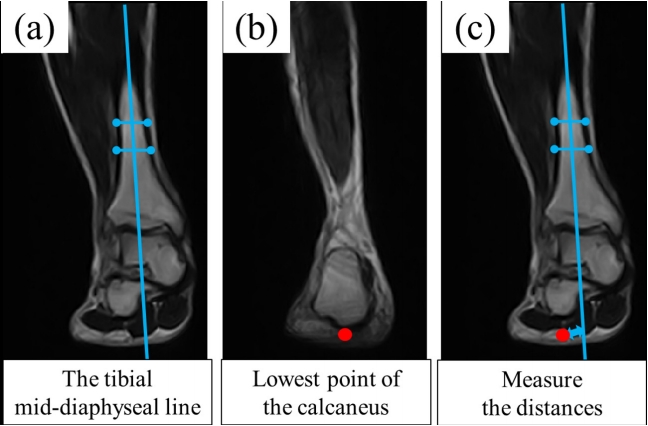
Measuring the hindfoot alignment view (HAV): (a) We drew two lines which connects two pairs of points on the cortex of the distal tibia. The lower line is set above the distal tibial spread adjacent to the ankle joint and the upper line approximately 2.0 cm above the lower line. Then, we drew the tibial mid-diaphyseal line which connects the midpoint of two lines. (b) We marked the lowest point of the calcaneus bone; and (c) we measured the HAV as the distance between the tibial mid-diaphyseal line to the lowest point of the calcaneus bone.
We analyzed NH, TH, MNP, and MTP values with reference to the methods of a previous study [2,24]. For measurement of NH (TH), coronal images of the foot were used. We chose the coronal image in which the lowest point of the navicular (talus) bone was visualized in order to determine the measuring point. Based on these images, the NH (TH) was measured as the distance from the floor to the lowest point of the navicular (talus) bone <Figure 2>.
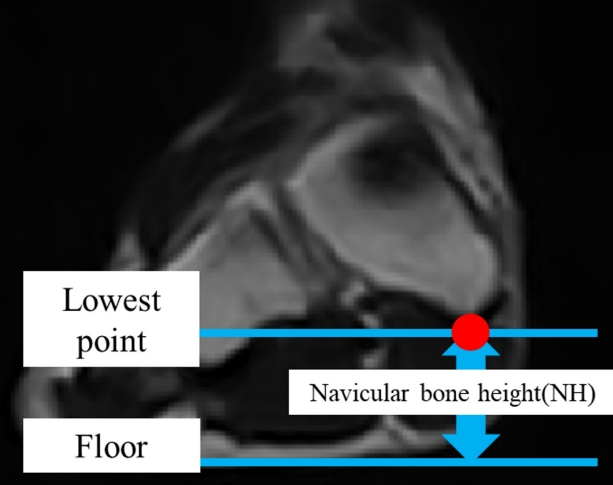
Measuring the navicular bone height (NH). We measured the NH as the distance from the floor to the lowest point of the navicular bone.
For measurement of MNP (MTP), axial images of the foot were used. First, we chose the axial image in which the head of the fifth metatarsal bone was visualized, as well as the axial image in which the most caudal point of the calcaneus bone was visualized. Based on these two images, the baseline for measurement of MNP (MTP) was determined <Figure 3> (a). Finally, the MNP (MTP) was measured as the distance from the baseline to the most medial point of the navicular (talus) bone <Figure 3> (b).
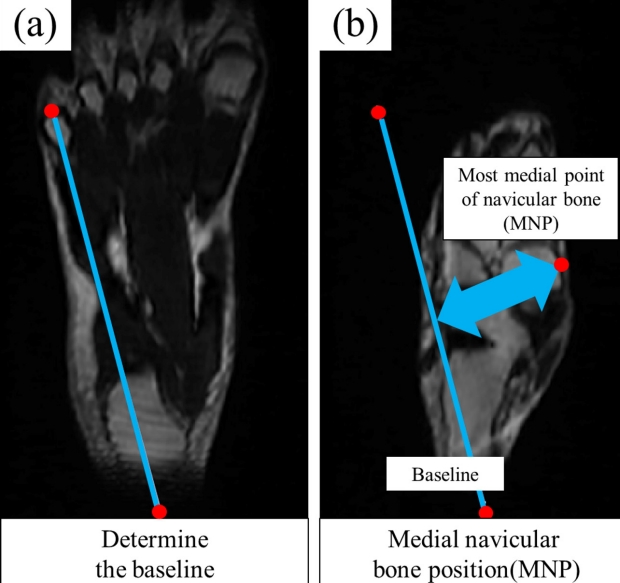
Measuring the medial navicular bone position (MNP): (a) First, we determined the baseline for measurements of MNP, which connects the most caudal point of the calcaneus bone and the head of the fifth metatarsal bone, and (b) we measured the MNP as the distance between the baseline and the most medial point of the navicular bone.
Calculation of Navicular and Talus Bone Position Changes
We calculated changes in the HAV, NH, TH, MNP, and MTP (ΔHAV, ΔNH, ΔTH, ΔMNP, and ΔMTP) between the NL and FW conditions (FW-NL).
The total weight-bearing response of the navicular and talus bones can be represented by both the distance and the direction. In this study, distance was represented using the total positional changes of the navicular and talus bones (∆TPCN, ∆TPCT), which is a combination of the vertical and medial displacements of these bones. ∆TPCN and ∆TPCT were calculated from vertical and medial displacements using the Pythagorean theorem, as follows: [2]
Direction was represented using the total positional angle changes of the navicular and talus bones (TPACN, TPACT), which is the ratio of the vertical-to-medial displacements of these bones. TPACN and TPACT were estimated using these equations: [2]
Statistical Analyses
Measurements for HAV, NH, TH, MNP, MTP, ΔHAV, ΔNH, ΔTH, ΔMNP, ΔMTP, ∆TPCN, and ∆TPCT are presented in millimeters. TPACT and TPACN are presented in degrees (°). We used the Shapiro-Wilk test to confirm the normality. Normality was not observed in the HAV alone on NL condition when a medial heel wedge was used. However, analysis of variance (ANOVA) is a robust statistic [25,26]; thus, we performed a two-way (two loading conditions [NL and FW]×two insole types [flat insole and medial heel wedge]) repeated-measures ANOVA for the HAV, NH, TH, MNP, and MTP. If significant interactions were found, the Bonferroni test was performed as a post hoc test for the NH, TH, MNP, and MTP and non-parametric Wilcoxon signed-rank tests was performed as a post hoc test for HAV. All statistical analyses were conducted using SPSS software, version 26.0, for Windows (IBM SPSS Japan Inc., Japan).
Results
<Table 1> shows the HAV, NH, TH, MNP, and MTP values under NL and FW conditions. HAV showed a significant loading conditions×insole interaction (F = 7.51; P = 0.01; η2 = 0.24). Under both NL and FW conditions, the HAV was significantly smaller on the medial heel wedge than on the flat insole (NL, P < 0.01; FW, P < 0.01). Additionally, NH showed a significant loading conditions×insole interaction (F = 12.61; P < 0.01; η2 = 0.35). Under the NL condition, no significant differences were observed between any insole types (P = 0.72). Under the FW condition, the NH was larger on the medial heel wedge than on the flat insole (P < 0.01). No significant interactions were observed for TH, MNP, or MTP (TH, F = 2.80, P = 0.11, η2 = 0.11; MNP, F = 3.56, P = 0.07, η2 = 0.13; and MTP, F = 2.23, P = 0.15, η2 = 0.09).

The position of foot arch bones in non-loading (NL) and full weight-bearing (FW) conditions. (n =25)
<Table 2> shows the ΔTPCN, ΔTPCT, TPACN, and TPACT. The ΔTPCN was significantly smaller on the insole with the medial heel wedge than on the flat insole (P < 0.01). No significant differences were observed for the ΔTPCT, TPACN, or TPACT (ΔTPCT: P = 0.07, TPACN: P = 0.46, and TPACT: P = 0.70).
Discussion
In our study, we evaluated the effects of a medial heel wedge on the weight-bearing response of hindfoot valgus and the total weight-bearing responses of the navicular and talus bones using pMRI. The present study contains salient findings that require discussion. First, under both NL and FW conditions, the HAV was smaller on the medial heel wedge than on the flat insole. Second, under the FW condition, the NH was larger on the medial heel wedge than on the flat insole. Finally, the ΔTPCN was significantly smaller on the medial heel wedge than on the flat insole.
Our results showed that a medial heel wedge reduced HAV values under both NL and FW conditions, indicating that the use of a medial heel wedge redirects the reaction forces acting on the plantar foot from a more lateral to a more medial location. Kirby et al. theoretically reported that redirecting the reaction forces acting on the plantar foot from a more lateral to a more medial location would decrease the hindfoot valgus moment [27]. Therefore, the use of a medial heel wedge may reduce the hindfoot valgus moment [28,29]. Excessive hindfoot valgus and hindfoot valgus moments have been linked to a risk of lower-limb overuse injuries [30,31]. Our findings indicate why the prescription of a heel wedge may be effective for the management of musculoskeletal disorders of the lower limb.
Furthermore, our results showed that when the heel wedge is inserted, NH increased under the FW condition and ΔTPCN decreased. It means that the use of a medial heel wedge plays a role in limiting the ΔTPCN by increasing the NH under the FW condition. Previous studies have reported that the movement of a hindfoot valgus correlates with the movements of the navicular and talus bones [2]. Therefore, a change in ΔTPCN (i. e., ΔTPCN on medial heel wedge condition - ΔTPCN on flat insole condition) may be caused by a change in ΔHAV (i.e., ΔHAV on medial heel wedge condition - ΔHAV on flat insole condition). We examined the relationship between the amount of change in ΔHAV (the average ± SD values was -0.40 ± 0.72) and the amount of change in ΔTPCN (the average ± SD values are in Table 2) using a Pearson’s correlation coefficient across all subjects, without finding a significant correlation (r = 0.04, P-value = 0.84). This result suggests that other factors, such as changes in plantar foot pressure due to the medial heel wedge, may limit the ΔTPCN [9]. Some previous studies have reported that increased mobility of the navicular bone is related to a risk of lower limb injuries [8,32]. Therefore, stabilization of the total weight-bearing response of the navicular bone by the prescription of a medial heel wedge may be effective for management of musculoskeletal disorders of the lower limb.
Our results also showed that the use of a medial heel wedge did not affect the TPACN nor the TPACT. When an axial load is applied, the rotation of the talonavicular joint around the subtalar joint axis has been reported to occur simultaneously with the weight-bearing response of the hindfoot valgus [33]. In addition, the navicular and talus bones slide down the subtalar articular surfaces as a rigid unit [33]. Then, the talus bone pushes out the navicular bone vertically and medially [33]. Based on this information, it is possible that the TPACN and TPACT could be affected by the subtalar joint axis location[2,27,33,34] and the talonavicular joint alignment [33]. Our results indicate that the use of a heel wedge may not change these structures, which may explain why the use of a medial heel wedge did not affect the TPACN nor the TPACT in our study.
This study had a few limitations. The present study was conducted only in healthy adult males, though age, gender, and foot function may also affect the weight-bearing response of foot-arch bones [8,32,35-37]. Further, we measured only the right foot of participants. The characteristics of the foot, such as the dominant leg, may affect our result [38]. Therefore, we should examine the effects of these factors in future studies.
We applied only one heel wedge and flat insole to clarify the effects of a medial heel wedge on the weight-bearing response of hindfoot valgus and the total weight-bearing responses of the navicular and talus bones. The participants’ foot morphologies may vary, and the pattern of combination of insole types and foot morphology may affect our results [39-41]. The relationship between the foot characteristics and the insole type should be examined in future studies. In contrast, several previous studies reported the effectiveness of a medial heel wedge similar in shape to the one we used [10,42-45]. We believe that these findings support our study.
We performed an MRI immediately after the participants wore the insole; hence, our results could have indicated the temporary effect of a medial heel wedge. Conversely, we could not consider the effects of acclimatization of the insole insertion and alignment over time. The effects of acclimatization of the insole insertion and alignment over time need to be discussed in future studies [46].
Moreover, we could not study the effects of medial heel wedge on the navicular and talus bone positions during exercise because measuring the weight-bearing responses of foot-arch bones during exercise has been challenging. To study the effects of medial heel wedge on the navicular and talus bone positions during exercise in future studies would be more realistic knowledge for clinical management [23]. However, we believe that our results are significant for the management of musculoskeletal injuries.
Conclusions
In conclusion, the present study suggested that a medial heel wedge decreases HAV values under both NL and FW conditions and stabilizes the total weight-bearing response of the navicular bone.
Acknowledgements
This work was partially supported by JSPS KAKENHI [Grant Number 19H05730].
Notes
The authors declare no conflict of interest.
